For years, the gut microbiome has been discussed in broad, sometimes vague terms, such as digestive comfort, immune support, and general “gut health.” While those functions matter, they’ve often kept microbiome science parked in the wellness category rather than the medical one.
That framing is starting to change.
A growing body of research suggests the gut microbiome plays a more direct and measurable role in metabolic health. Rather than acting only through digestion or inflammation, gut bacteria produce specific metabolites (small, bioactive molecules) that influence how the body regulates glucose, stores fat, and responds to insulin.
New research has brought renewed attention to this shift, describing how gut-derived molecules can alter liver metabolism and insulin signaling, pathways central to obesity and type 2 diabetes. The implication is significant: the microbiome may be influencing metabolic disease risk well before traditional markers like elevated blood sugar or weight gain appear.
This article explores what microbiome metabolites are, how they affect metabolic control, and why they are increasingly viewed as a promising, though still emerging, tool in disease prevention.
How Gut Bacteria Communicate With the Body
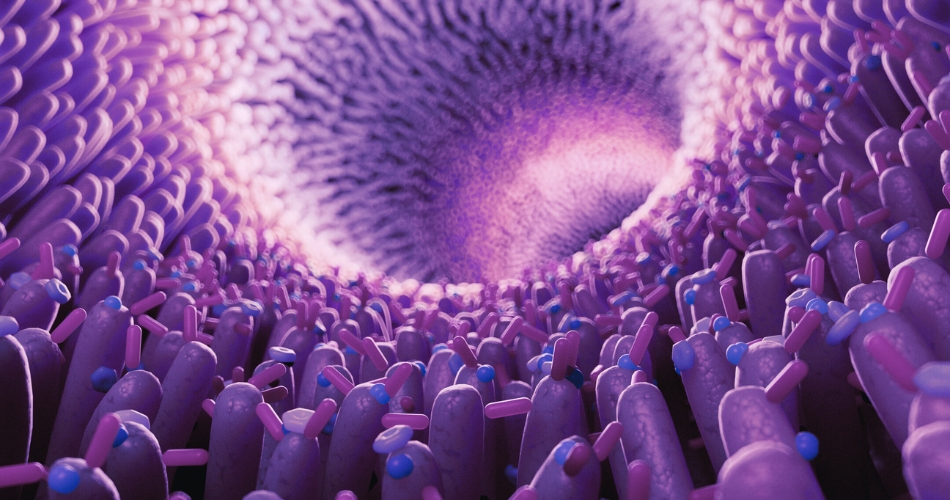
Microbiome metabolites are bioactive compounds produced when gut bacteria break down components of the diet, particularly fibers, proteins, and fats that human enzymes cannot fully process on their own.
Some of the most studied examples include short-chain fatty acids (SCFAs) such as acetate, propionate, and butyrate; bile acid derivatives created through microbial modification; and metabolites derived from amino acids. Unlike nutrients that remain largely within the digestive tract, these molecules can enter circulation and act as signaling agents throughout the body.
Once produced, microbiome metabolites interact with receptors in organs such as the liver, pancreas, adipose tissue, and even the brain. Through these pathways, they influence insulin sensitivity, inflammatory signaling, appetite regulation, and energy storage. Importantly, these effects are not uniform. They depend on the composition of the microbiome, dietary patterns, and underlying metabolic health.
This signaling role is what has moved microbiome research out of the realm of correlation and toward mechanism.
Why the Liver Is Central to the New Microbiome Story
The liver sits at the crossroads of metabolism. It regulates blood glucose levels, processes lipids, and plays a central role in insulin responsiveness. It is also one of the first organs exposed to gut-derived metabolites through portal circulation, making it especially sensitive to microbiome signaling.
Recent findings suggest that certain microbial metabolites can alter hepatic glucose production, either improving or impairing insulin sensitivity depending on their profile and concentration. Others appear to influence fat accumulation in the liver, a key driver of insulin resistance and metabolic dysfunction.
This gut–liver axis helps explain why differences in microbiome composition are associated with varying risks of obesity, type 2 diabetes, and fatty liver disease. Rather than acting downstream of disease, microbiome metabolites may be shaping metabolic trajectories earlier than previously recognized.
Implications for Obesity and Type-2 Diabetes Prevention
Obesity and type-2 diabetes are increasingly understood as disorders of metabolic signaling, not simply the result of excess calories or insufficient willpower. Insulin resistance often develops gradually, driven by complex interactions between genetics, diet, inflammation, and organ function.
Microbiome metabolites may play a role in this early phase. Research suggests they can contribute to insulin resistance before fasting glucose or A1C levels rise, and may influence weight gain independent of total caloric intake. In that sense, they offer a window into metabolic risk that precedes overt disease.
This perspective supports a preventive approach focused on metabolic health rather than weight alone; one that looks at how the body processes energy, responds to insulin, and maintains flexibility under metabolic stress.
From Probiotics to Metabolic Medicine
Early enthusiasm around the microbiome often centered on probiotics and generalized dietary advice. While these interventions can be beneficial for some individuals, they rarely addressed specific metabolic mechanisms.
Current research is more targeted. Scientists are identifying individual metabolites, mapping cause-and-effect pathways, and exploring how diet, microbiome composition, and host metabolism interact. The goal is not to promote a one-size-fits-all supplement, but to understand which microbial signals matter, and under what conditions.
As a result, microbiome science is increasingly being framed as part of metabolic medicine rather than wellness culture. This shift mirrors what has happened in other areas of prevention, where broad lifestyle advice has been complemented by more precise biological insight.
What Patients and Clinicians Should Take From This
It is important to be clear about what this research does (and does not) mean.
It does not suggest that a single supplement can prevent diabetes, or that microbiome testing replaces standard metabolic screening. Clinical translation remains in its early stages, and well-designed trials are still needed.
What it does suggest is that diet quality matters at a molecular level, that early metabolic changes may be detectable before disease develops, and that future prevention strategies may combine nutrition, microbiome modulation, and metabolic monitoring in more integrated ways.
For clinicians, this research reinforces the importance of looking beyond surface measures. For patients, it underscores that metabolic health is shaped by complex biological systems—not just calories or weight.
A New Role for the Microbiome in Prevention
Gut microbiome metabolites are emerging as meaningful regulators of liver metabolism and insulin response, shifting the microbiome conversation from generalized “gut health” to evidence-based metabolic prevention.
As obesity and diabetes continue to rise globally, understanding, and eventually learning how to influence, these microbial signaling pathways may become an important part of preventive care. The challenge now is translating promising biology into practical, safe, and equitable strategies that improve long-term metabolic health.
In that sense, the microbiome is no longer a side note. It is becoming part of the core conversation about how metabolic disease begins, and how it might be prevented earlier than ever before.
Conclusion
The emerging science around gut microbiome metabolites marks an important shift in how obesity and type-2 diabetes are understood, and potentially prevented. Rather than viewing the microbiome as a peripheral player in digestion or immunity, researchers are now mapping clear biochemical pathways through which gut-derived molecules influence liver metabolism, insulin sensitivity, and energy regulation.
This work reframes metabolic disease as a process that begins well before traditional warning signs appear. If gut-derived signals help shape insulin resistance and fat accumulation early, prevention may need to focus less on reacting to disease and more on maintaining metabolic signaling integrity over time.
For now, these findings reinforce a familiar but evolving message: prevention is most effective when it is grounded in biology, not buzzwords. As microbiome research continues to mature, its role in metabolic medicine is likely to become more precise, more actionable, and more central to how clinicians think about long-term cardiometabolic health.
Sources
Harvard T.H. Chan School of Public Health





